-
Recent Posts
Archives
- October 2022
- August 2022
- May 2022
- March 2022
- January 2022
- December 2021
- September 2021
- July 2021
- June 2021
- May 2021
- April 2021
- February 2021
- January 2021
- November 2020
- October 2020
- September 2020
- June 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- June 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- December 2014
- June 2014
- May 2014
- April 2014
- November 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- March 2013
- January 2013
- November 2012
- October 2012
- July 2012
- December 2011
- November 2011
- October 2011
- September 2011
- August 2011
- July 2011
- June 2011
- May 2011
- April 2011
- March 2011
- February 2011
- January 2011
- December 2010
- November 2010
Categories
Meet the NorthStar VETS Team: Kirk Herrmann, DVM (Practice Limited to Dentistry and Oral Surgery)
Kirk Herrmann, DVM is a doctor in the Dentistry and Oral Surgery service at NorthStar VETS. In this video, he talks about what drew him to veterinary dentistry, the importance of oral health, and the type of case that has the greatest impact for him.
How Dr. Herrmann got into Veterinary Medicine
We caught up with Dr. Herrmann, who was checking on a patient before heading to a procedure, where he told us about the kind of work he does. “Primarily, I work on dental cases such as extractions, root canals associated with fractures, and things like that, but I also do maxillofacial surgery, including oral tumors and jaw fractures. I repair those and get those animals back to working order.”
“The reason I wanted to get into veterinary medicine is because I was surrounded by animals as a child. We had horses, dogs, cats, pot-bellied pigs and everything under the sun. To me, there was no other profession I wanted to do! As far as becoming a veterinary dentist, that came later in life. I realized I liked surgical things where I could fix problems, and I also knew that I liked to be focused. Veterinary dentistry and oral surgery allows me to focus on a particular area of the body. What I love about being a veterinary dentist is that every day I come in to something that is new. No two mouths are the same, no two issues are the same, and I love seeing pets come back two weeks later after relatively extensive oral surgery and doing fantastic.”
“I went to veterinary school at the University of Florida College of Veterinary Medicine. From there, I did a rotating internship at the Specialty Center of Delaware, and I did my residency under the mentorship of Drs. Mark Smith and Kendall Taney at the Center for Veterinary Dentistry and Surgery in Gaithersburg, Maryland.”
The importance of veterinary dentistry
“Sometimes we don’t know there’s a problem until it’s too late. Part of how we deal with that is being proactive. That means home care, yearly dental cleanings under anesthesia, and also diets including what is good and bad to chew on because a lot of the things that I see are preventable. Sometimes these fractured teeth and severe periodontal disease are things we could nip in the bud earlier with appropriate home care and regular dental cleanings.”
“Dental health is something that for a period of time in veterinary medicine, and even sometimes in human medicine, is overlooked. We have to understand that everything that happens in the mouth whether that’s inflammation of infection affects the rest of the body. Not only that, but it’s something that gives a patient general malaise, makes them tired, and other nondescript symptoms. Oral health is important to them for managing other aspects of their disease, and if they have oral health problems, it’s often exacerbating pre-existing conditions or causing that general malaise or lethargy that you don’t realize is a problem for your pet until we fix it.”
The type of case that has the greatest impact on Dr. Herrmann
“A case that comes to mind that really impacted me was more about the client patient relationship where a young dog was suffering from a lot of oral pain. The client was a very diligent person and a wonderful caretaker. When she identified this problem, she came to us and we unfortunately gave a diagnosis of a chronic ulcerative disorder in the pet’s mouth which often requires extensive extractions. It was a bit of a blindside to that client and even for us because it was kind of on the fence. When I tell someone a diagnosis that’s poor, but I’m able to fix it, having that positive outcome in the end and that relationship that we’ve built up with the client over time is worth it. When the client initially doesn’t see the problem, but in the end is very happy with their decision, that is always impactful to me.”
https://www.youtube.com/watch?v=LOJmlAGDxkA
Learn more about the Dentistry and Oral Surgery service at NorthStar VETS.
Kirk Herrmann, DVM (Practice Limited to Dentistry and Oral Surgery)
 Dr. Herrmann is a Bucks County native who obtained his degree in Animal Science from Delaware Valley University. He then moved south where he pursued his childhood dream at the University of Florida College of Veterinary Medicine. There, he obtained his doctorate. He continued his education with a rotating internship at The Veterinary Specialty Center of Delaware and a 3-year residency at the Center for Veterinary Dentistry and Oral Surgery in Gaithersburg, Maryland.
Dr. Herrmann is a Bucks County native who obtained his degree in Animal Science from Delaware Valley University. He then moved south where he pursued his childhood dream at the University of Florida College of Veterinary Medicine. There, he obtained his doctorate. He continued his education with a rotating internship at The Veterinary Specialty Center of Delaware and a 3-year residency at the Center for Veterinary Dentistry and Oral Surgery in Gaithersburg, Maryland.
Dr. Herrmann has a strong interest in providing healthy and functional mouths for our pets through surgery, interceptive procedures and client education. In his spare time he enjoys the outdoors, gardening, cooking and relaxing with his large extended family.
Posted in Pets, Veterinary Medicine
Tagged Dentistry, Kirk Herrmann, NorthStar VETS, Veterinary
Leave a comment
Domestic Companion Animals and COVID-19
Excerpted from the New Jersey Department of Health document published June 8
We are still learning about how the virus that causes COVID-19 can affect animals. A small number of pets (cats and dogs) have been confirmed to be infected with the virus that causes COVID-19, mostly after close contact with a person with COVID-19. Some pets did not show any signs of illness, but those pets that did get sick all had mild disease that could be taken care of at home. None of the pets have died.
Based on the limited information available now, the risk of pets spreading COVID-19 to people is considered to be low. There is no reason to abandon or surrender pets that have been confirmed positive for the virus that causes COVID-19.
Routine testing of companion animals for COVID-19 is currently not recommended. Tests for COVID-19 in animals should only be considered for animals with COVID-19 symptoms and that have been exposed to a person with COVID-19.
Posted in Pets, Veterinary Medicine
Tagged Coronavirus, COVID-19, New Jersey Department of Health, NJDOH, NorthStar VETS
Leave a comment
Updates To Our Covid-19 Hospital Protocols
On Monday, June 8, 2020, NorthStar VETS will begin our phase of reopening our hospitals to the public. We understand that the safety of our clients and staff is our highest priority, and we will continue to follow safety protocols outlined by the state.
As you pull into our facility please call (609) 259-8300 from your vehicle to announce your arrival, listen for instructions, and wait to be called in. With the warmer weather heating up, we will allow one client with their pet to enter the building. Pet parents must wear a mask or face covering as they enter and a staff member will swiftly escort them to a private exam room. If you do not have a face covering, one will be provided.
Plexiglass shields have been installed at all of our check-in and check-out desks along with touchless credit card machines. We’ve added floor decals to our waiting areas to enforce the 6′ apart distancing rule. We ask that everyone in our hospital maintain social distancing practices and utilize the hand sanitizing dispensers located throughout the facility. Clients that fail to comply with our COVID-19 protocols will be denied services.
For pet euthanasias, both of our Brick and Robbinsville comfort rooms have doorways leading to the outside and we will continue to use them. There is no limitation on the number of family members that can be present with their beloved companion animal during euthanasia.
Lastly, we will continue our curbside check-in and emergency triage for all locations. For pet parents wishing to safely remain in their vehicle, our staff will come out to receive your pet and communicate via phone to limit face-to-face contact.
We thank you for your patience and understanding and hope that you are staying healthy and safe during this time.
The NorthStar VETS Team
Surgery Success Opie
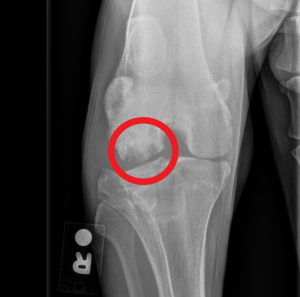
 Opie is a two-year-old Great Dane recently referred to NorthStar VETS. Opie had been favoring his right rear limb for a few months and then became acutely more lame after playing outside with his housemate. Initial radiographs and exam suggested rupture of his ACL. However, when another X-ray of the knee was taken we became suspicious of a condition known as Osteochondritis Dessicans (OCD). This condition typically occurs in young growing dogs and is due to abnormally developing cartilage and bone. As a result a weak spot forms in the joint causing pain and lameness.
Opie is a two-year-old Great Dane recently referred to NorthStar VETS. Opie had been favoring his right rear limb for a few months and then became acutely more lame after playing outside with his housemate. Initial radiographs and exam suggested rupture of his ACL. However, when another X-ray of the knee was taken we became suspicious of a condition known as Osteochondritis Dessicans (OCD). This condition typically occurs in young growing dogs and is due to abnormally developing cartilage and bone. As a result a weak spot forms in the joint causing pain and lameness.
 Dr. Daniel Stobie and Dr. Kelly Johnson of the NorthStar VETS Surgery team performed an OATS procedure (Osteochondral Autograft Transfer System) on Opie’s right stifle. This is a procedure where a plug of normal cartilage and bone is collected from another site in the joint. The plug is then placed in the site of weakened cartilage to help restore and heal the joint surface. The procedure went well and Opie will be seeing our Rehabilitation Department to help him heal and strengthen his new joint!
Dr. Daniel Stobie and Dr. Kelly Johnson of the NorthStar VETS Surgery team performed an OATS procedure (Osteochondral Autograft Transfer System) on Opie’s right stifle. This is a procedure where a plug of normal cartilage and bone is collected from another site in the joint. The plug is then placed in the site of weakened cartilage to help restore and heal the joint surface. The procedure went well and Opie will be seeing our Rehabilitation Department to help him heal and strengthen his new joint!
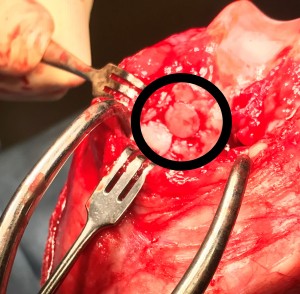
Figure 1: The circular piece of bone in the center of the image was removed from a nearby piece of bone and inserted into the defect in the knee.
Learn more about the Surgery service at NorthStar VETS.
Daniel Stobie, DVM, MS, DACVS – Chief of Staff
 A New Jersey native, Dr. Stobie completed his undergraduate work at Cook College/Rutgers University and is a 1990 cum laude graduate of the University of Missouri-College of Veterinary Medicine. He completed an internship in small-animal medicine and surgery at the Angell Memorial Animal Hospital in Boston, then went on to complete a three-year surgical residency at the University of Minnesota and earn a Master’s Degree in Veterinary Surgery, Radiology, and Anesthesia in 1994. Dr. Stobie became a Diplomate of the American College of Veterinary Surgeons in 1995. In 2007, he completed the mini-MBA certificate program at the Rutgers School of Business. Learn more about Dr. Daniel Stobie.
A New Jersey native, Dr. Stobie completed his undergraduate work at Cook College/Rutgers University and is a 1990 cum laude graduate of the University of Missouri-College of Veterinary Medicine. He completed an internship in small-animal medicine and surgery at the Angell Memorial Animal Hospital in Boston, then went on to complete a three-year surgical residency at the University of Minnesota and earn a Master’s Degree in Veterinary Surgery, Radiology, and Anesthesia in 1994. Dr. Stobie became a Diplomate of the American College of Veterinary Surgeons in 1995. In 2007, he completed the mini-MBA certificate program at the Rutgers School of Business. Learn more about Dr. Daniel Stobie.
Kelly Johnson, DVM, MS, DACVS Dr. Kelly Johnson is a Vermont native who received her undergraduate degree from the University of Richmond in 2002. She earned her veterinary degree from Michigan State University in 2006. After graduation she completed a small animal rotating internship at the Hope Advanced Veterinary Center in Vienna, VA followed by her surgical residency at the Virginia-Maryland College of Veterinary Medicine. During her residency she also completed a Master’s Degree in Biomedical and Veterinary Sciences. Dr. Johnson practiced as a small animal surgeon in northern NJ for nine years before joining NorthStar VETS in 2020.
Dr. Kelly Johnson is a Vermont native who received her undergraduate degree from the University of Richmond in 2002. She earned her veterinary degree from Michigan State University in 2006. After graduation she completed a small animal rotating internship at the Hope Advanced Veterinary Center in Vienna, VA followed by her surgical residency at the Virginia-Maryland College of Veterinary Medicine. During her residency she also completed a Master’s Degree in Biomedical and Veterinary Sciences. Dr. Johnson practiced as a small animal surgeon in northern NJ for nine years before joining NorthStar VETS in 2020.
Dr. Johnson is trained in the tibial tuberosity advancement (TTA) and lateral extracapsular suture techniques for cranial cruciate ligament disease. Outside of work she enjoys paddle boarding, yoga, downhill skiing, traveling, attending country concerts and watching the New York Rangers.
 Rosalie LoScrudato, DVM, CVA, CCRP
Rosalie LoScrudato, DVM, CVA, CCRP
Certified Veterinary Acupuncturist, Certified Canine Rehabilitation Practitioner
Dr. LoScrudato received her undergraduate degree from Cook College, Rutgers University, and graduated from the University of Missouri College of Veterinary Medicine in 1990. After graduation, Dr. LoScrudato returned to New Jersey and practiced small animal medicine for 17 years, developing an interest in emergency and critical care medicine. She joined NorthStar VETS in 2007 as an emergency clinician.
Dr. LoScrudato earned her certification in veterinary acupuncture in 2009 from the Chi Institute. Dr LoScrudato started the Acupuncture service at NSV in 2009, giving our hospital another avenue to improve our patients’ comfort and function. Beginning in 2011, she transitioned from our ER department and dedicated her time to building the rehabilitation and pain management service at NSV along with Dr Pamela Levin. She completed her certification as a canine rehabilitation practitioner from the University of Tennessee College of Veterinary Medicine in 2012. Dr LoScrudato was certified in companion animal pain management in March 2015. She considers her greatest achievements her four beautiful children. Dr LoScrudato enjoys music, spending quality time with her children, and fishing.
COVID-19 Testing for Pets
The confirmation of COVID-19 in a Tiger at a New York zoo raised concerns among pet parents regarding the possibility of transmitting the virus to domestic cats. This information from the New Jersey Veterinary Medical Association breaks down the facts:
- There have been no reports of pets or livestock becoming ill with COVID-19 in the United States. At this time, there is no evidence that domestic animals, including pets and livestock, can spread COVID-19 to people.
- The isolated case of a COVID-19 positive Tiger in New York is being monitored and additional information is needed before complete conclusions can be drawn.
- If your pet shows respiratory or gastrointestinal signs, your veterinarian will test for more common pathogens and conditions. With “Stay at Home” orders in place, there is a possibility pets may be exposed to increased respiratory irritants (aromatherapy products, household cleaners and disinfectants) or have greater opportunities for dietary indiscretion.
- Routine testing of domestic animals for COVID-19 is not currently being recommended by the AVMA, CDC, USDA, or the American Association of Veterinary Laboratory Diagnosticians (AAVLD).
- If you become ill with COVID-19, it is recommended to have another member of your household care for pets until you are recovered. If this is not possible, contact with pets should be kept to a minimum, and sick individuals should wash their hands thoroughly before and after contact with pets. This may be difficult for pets that need affection and don’t understand the situation.
Have an emergency plan in place in the event you are hospitalized:
- Identify a trusted pet caregiver, or contact your local veterinarian or potential boarding facilities to see if they can offer safe shelter for your pet during a health emergency.
- Make sure pet identification and microchip registration is up to date.
- Record important information about your pet so that you can easily access it during an emergency.
- Put together a “Go Bag” for each pet with basic food, supplies, medicine, identification, a list of emergency contacts, your veterinarian’s contact information, and vaccination proof.
- Ensure all medications are documented with dosages and administering instructions.
Posted in Pets, Veterinary Medicine
Tagged Coronavirus, COVID, COVID-19, New Jersey Veterinary Medical Association, NJVMA, NorthStar VETS, pets
Leave a comment
Rabbit Hemorrhagic Disease Virus Frequently Asked Questions
What is Rabbit Hemorrhagic Disease?
Rabbit Hemorrhagic Disease Virus (RHDV) is a serious viral disease that may cause a high rate of infection and death in rabbits. It does not cause disease in humans or animals other than rabbits. It is caused by a Calicivirus, which can survive for weeks in the environment, and can be spread over short distances on objects such as articles of clothing, and therefore can be spread easily and rapidly.
Why is it Significant that RHDV2 has Been Found in New Jersey?
As of 03/19/2020, USDA has identified an isolated event of 13 confirmed cases of RHDV2 that can be linked to a veterinary hospital in New York City. All cases were from New York and there are no confirmed cases at this time in New Jersey.
There are several types of RHDV viruses. RHDV outbreaks, with original strains of the virus (not RHDV2), have been reported in pet rabbits in the US in 2000 (Iowa), 2001 (Utah, Illinois, New York), 2005 (Indiana), 2008 (Maryland) and 2010 (Minnesota). In these cases, only a single household or facility was involved, with no further spread. These short-lived, small outbreaks were controlled by isolation and cleaning. There was a single, isolated reported case of RHDV2 in Ohio back in September 2018 and there were no other cases seen in that area. That case was the only report until the reported cases recently in New York, which has also believed to be an isolated event. The virus reported recently in NYC is the newer strain, RHDV2. This new strain is able to infect a wider variety of rabbit species, to include wild rabbits such as cottontails and jackrabbits. The NY and NJ Department of Agriculture is working with state and federal agencies to conduct careful surveillance of wild rabbits in the area surrounding the confirmed case of RHDV2.
What Are the Symptoms of RHDV2?
Affected rabbits may die suddenly without symptoms or may have a fever or show neurologic signs such as incoordination, excessive excitement, convulsions, paddling, or paralysis prior to death. Most will appear to have difficulty breathing just before death and may have a bloody discharge from the nose. There also may be observable hemorrhages in the eye, blood in feces, and icteric skin coloration. Death usually occurs within 1 to 3 days. A few may have milder signs and survive, developing antibodies, but this is rare. There is a chronic form where jaundice, weight loss and lethargy give way to death after a few weeks. Rabbits can become infected with RHDV at any age, but young rabbits (less than 40-to-50 days old) experience only subclinical disease. However, the death rate is very high – between 40-100%. In recent Canadian outbreaks of RHDV2, the death rate was close to 90%. Infection with RHDV also causes lesions throughout internal organs and tissues, particularly on the liver, lungs and heart, resulting in the characteristic hemorrhaging and fatally rapid progression of the disease. Signs of RHD may be similar to septicemic pasteurellosis, severe septicemia from other causes presenting with secondary disseminated intravascular coagulation, poisoning, and heat exhaustion.
How Long Does it Take for a Rabbit Exposed to the Virus to Become Ill?
The time from virus exposure to symptoms (incubation period) is very short, within 16 to 48 hours. Fatalities are usually occurring within 2-9 days after infection. The infectious period may last up to one month.
How is the Virus Spread?
Infected rabbits pass on the virus through any body fluid, including urine, feces, or fluid from the eyes nose or mouth. The virus survives outside of the body, so can be found on rabbit fur, bedding or anything the infected rabbit touches. The virus can live for weeks in wet organic material such as dirty bedding. It can be passed over short distances on clothing, shoes or hands. It can also be spread by flies and mosquitos. It is resistant to freezing and heat. Surviving rabbits are immune but can continue to pass virus for 42 days or more.
How is the Virus Treated?
There is no cure for RHDV. Rabbits that are not severely infected may be more likely to survive with supportive care such as fluids and assisted feeding.
Can my Rabbit be Vaccinated to Prevent This Disease?
Vaccines are available in places where the disease is widespread, such as Europe. After several outbreaks of RHDV2 occurred in British Columbia on the west coast of Canada from February to April 2018, the Canadian government issued emergency, provisional license to use this vaccine in specified affected areas only. There is no vaccine approved for use in the U.S.
How Can I Protect My Rabbit?
At this time, the virus has not been reported outside of the original isolated events. Since the virus can be carried on shoes, clothing, or hands, it is important to pay particular attention when coming home to your rabbit after you have visited locations where other rabbits have been. This would include pet stores, feed stores, shows, shelters, etc.
To Protect Your Rabbit:
- Change your clothes after handling or coming in contact with rabbits. Wash these clothes twice in hot water before you wear them around your rabbit.
- If you volunteer at a shelter in an area with an outbreak, wear protective clothing or a set of clothing and shoes that you wear only at the shelter. You may want to wear shoe covers or plastic bags over your shoes, secured with a rubber band. When you leave the shelter, remove and dispose of the covers before entering your car, making sure not to touch the outside of the bag. Launder these clothes separately from your other clothes in hot water twice.
- Take your shoes off and ask your guests to remove their shoes before entering your home.
- To disinfect shoes that may have been contaminated, place the shoes in a foot bath that contains one of the below disinfectants.
- Other items to be disinfected must be in contact with the disinfectant for at least ten minutes, during which time the disinfectant must remain wet. Merely spraying shoes with disinfectant and leaving them to dry is not effective.
- Use an effective disinfectant for this virus: bleach (1:10 dilution), potassium peroxymonosulfate (Virkon), accelerated hydrogen peroxide (Prevail, Accel, Rescue wipes or solution, and Peroxigard), parvoviricide disinfectant (Parvosol), or substituted phenolics (2% One-stroke Environ). You may wish to speak with your veterinarian about how to obtain these.
- Know your sources of hay and feed and if they are near areas of any outbreaks.
- Minimize insects in your home by installing window and door screens. Eliminate mosquitoes and flies from your home.
- If your rabbit(s) are housed outdoors, implement an insect control system, including additional screening/netting, insect catchers, professional insect control services, etc.
- Quarantine any new rabbit for at least 10-14 days or longer. Always handle quarantined rabbits last and keep all supplies for them separate from your other rabbits’ supplies.
How Can I Protect Other Rabbits?
- Following the procedures listed above to protect your own rabbit will also protect other rabbits by preventing spread of the virus.
- If you have a rabbit die suddenly, or die after demonstrating symptoms such as seizures, incoordination, difficulty breathing or a bloody discharge from the nose, it is essential that not bury the remains. Virus can live in the remains for months and become a source of infection to wild rabbits. Please take the remains to your rabbit’s veterinarian for a diagnosis, or contact the NJ Animal Health Diagnostic Lab at: jerseyvetlab.nj.gov
Download this information in PDF form.
Learn more about the Avian and Exotics service at NorthStar VETS.
 Andrea Winkel-Blair, DVM, MPH
Andrea Winkel-Blair, DVM, MPH
Dr. Winkel-Blair graduated from Michigan State University CVM in 2009 and completed her Masters in Public Health from the University of Minnesota in 2010. She went on to join the U.S. Army Veterinary Corps in 2009 where she was an active duty captain. After 4.5 years, she decided it was time for a change and left the Army for private practice. Dr. Blair was in private practice for about 1 year before she decided to go back for a residency in Avian medicine. She completed her Avian medicine and Surgery residency at Texas A&M University where she worked on all sorts of exotics, from big cats to hummingbirds. She spent a year at an avian & exotics exclusive specialty service in Columbus, OH before joining the staff at NorthStar VETS in Robbinsville, NJ.
Posted in Pets, Pets, Veterinary Medicine
Tagged Andrea Winkel-Blair DVM, NorthStar VETS, Rabbit Hemorrhagic Disease Virus, RHDV
6 Comments
Curbside Check In
Scheduled appointments will pull into our parking lot and call (609) 259-8300 to notify their arrival. Clients should have already completed their check-in paperwork online at northstarvets.com prior to the consult.
A masked/gloved staff member will greet the vehicle and review any check-in paperwork. When the appointment time is ready, a technician will escort the pet to the exam as the client waits in their vehicle.
Clients are not permitted to enter the building at this time. Exceptions are made for euthanasia appointments as that room has its own entrance.
The veterinarian will call the pet parent to discuss their findings/recommendations during the exam. Once the patient visit is complete, discharge instructions, prescriptions and payment will be managed by phone and/or at the vehicle as pets are returned to their owners.
The hospitals’ main entrances are now reserved for pet emergency triage.
Social distancing is our top priority, and we appreciate your cooperation with these changes to keep our staff, clients, and pets safe!
Coronavirus Information from NorthStar VETS
Dear Pet Parents,
As the Coronavirus (COVID-19) is an evolving topic for our clients, NorthStar VETS Medical Directors have reviewed multiple health organization recommendations. First and foremost, we are monitoring and taking precautions to protect you and your pets during what the World Health Organization (WHO) has declared as a pandemic. Below is important information on ways that NorthStar VETS continues to protect our community.
THE MOST IMPORTANT THINGS PET PARENTS SHOULD KNOW:
- According to the CDC, there is currently no known reason to believe that any animals, including pets in the US, can spread COVID-19.
- The CDC always recommends following everyday preventive actions to help prevent the spread of illness.
- As a rule, pet parents should practice good hygiene habits, including washing hands before and after handling pets/food/supplies and maintaining a clean environment
If you see any changes in your pet’s health condition, contact your family veterinarian.
NORTHSTAR VETS IS PUTTING THESE SAFEGUARDS IN PLACE:
- Continuing to maintain our clean and sterile environments while taking additional precautions for the safety of our clients
- Cleaning services/practices have been increased in high-traffic areas, and multiple hand-sanitizing stations have been
installed throughout our hospitals. - Furniture, counters, floors, door handles, exam rooms, and patient treatment areas are thoroughly (and frequently) disinfected.
- Our staff practices good hygiene by covering coughs and sneezes, not touching their faces, and not coming in close proximity to those feeling “under the weather.”
- Management encourages sick team members to stay home to help prevent the spread of illness.
HOW WE ARE IMPLEMENTING “SOCIAL DISTANCING”:
- Having clients fill out online forms ahead of time to minimize waiting in our lobby.
- Upon arrival, clients may call (609) 259-8300 from their vehicle to verbally check-in for their specialist consult.
- After check-in, clients may wait in their vehicles for their scheduled appointment until our staff is ready to escort the pet to an exam room. Exceptions are made for euthanasia appointments.
- Clients will be invoiced directly and given their pet’s prescriptions and discharge instructions.
- As always, clients may pay their invoice on our secure online checkout.
- Pet prescriptions may be (re)filled at our online pharmacy at northstarvets.com.
- Meetings/lectures/tours have been cancelled and we’ve implemented a strict, corporate “no-handshake” policy.
We know that anxious clients have scheduled appointments with our veterinary specialists, and we are happy to discuss your concerns by contacting (609) 259-8300. Please know that NorthStar VETS remains steadfast and confident in our ability to navigate this uncertain period and are doing all we can to protect you, your pets and our employees.
Sincerely,
Daniel Stobie, DVM, MS, DACVS, Chief of Staff
Kimberly Hammer, VMD, DACVIM, Medical Director, Robbinsville
Stacey Rebello, DVM, MS, Director of Emergency Services
Nancy Vail, DVM, Medical Director, Maple Shade
Benjamin Donati, VMD, Medical Director, Brick
NOTE: Additional resources may be found on the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) websites.
Hemodialysis for Pets
Yes, it’s true. Dogs and cats are able to benefit from hemodialysis just as people are. The use of hemodialysis in veterinary medicine is a little different compared to people but the basic principles are the same. Here we will explain the basics of hemodialysis as well as the indications for this treatment in dogs and cats.
What is the normal function of the kidney?
The kidneys (there are usually two – left and right) are organs located in the abdomen. Their primary job is to filter the blood, removing by-products of metabolism and toxins from the body. Kidneys also participate in the following:
- Keeping blood electrolyte and mineral concentrations in the normal range
- Red blood cell production
- Blood pressure control
- Regulation of water content in the body
 What is hemodialysis?
What is hemodialysis?
Hemodialysis is the movement of blood through a filter and cleaning the blood of toxins that build up in the body when the kidneys are not working effectively. The filter is located outside of the body and the blood is moved through a blood circuit.
Is a special catheter used?
The use of a hemodialysis catheter facilitates the movement of blood outside of the body. This catheter is larger than regular intravenous catheters allowing high flow rates of blood. In most pets, placement of the hemodialysis catheter is in the right jugular vein. A majority of dogs and cats will have placement of the catheter under general anesthesia. X-rays confirm proper placement of the catheter. Sterility is of utmost importance to reduce the risk of infection. The hemodialysis doctors place these catheters with the same sterility as a surgeon uses when performing surgery.
Why would my pet need hemodialysis?
Many of us have had a family member or friend treated with hemodialysis, or have seen movies or TV programs showing people getting hemodialysis. Hemodialysis conjures an image of people living the rest of their life hooked up to a machine. In this situation, these people have end-stage kidney disease caused by chronic illness such as diabetes or high blood pressure. As these people have no hope of regaining normal kidney function, they will remain dependent on hemodialysis for the remainder of their lives. Some people may be candidates for a transplant but for most, hemodialysis (or chronic peritoneal dialysis) remains the only option.
In veterinary medicine, cost and considerations of quality of life for pets limit the use of hemodialysis for treatment of chronic kidney disease. Most often, veterinarians use hemodialysis to treat acute kidney disease. Acute kidney disease differs from chronic kidney disease for many reasons. Of these differences, reversibility of the underlying process is the most important, especially when we are recommending hemodialysis to treat a patient with acute kidney disease. Long-standing damage to the kidney leading to loss of the normal kidney function of filtering the blood leads to illness. Various diseases can lead to chronic damage of the kidney tissue. In response to this damage, scar tissue builds up, leading to irreversible loss of kidney function. These chronically damaged kidneys have little to no ability to repair themselves.
Acute kidney disease differs in that there is a chance of repair and return to normal function. Acute insults to the kidney can lead to acute kidney injury. The insult could be an infection (e.g. leptospirosis), a toxin (e.g. ethylene glycol, non-steroidal anti-inflammatory drugs), and/or decreased blood flow, to name a few. Once damaged, the kidney’s function declines and the pet starts to feel sick. Treatment of the underlying disease can eliminate the ongoing damage. The kidney then has a chance at repairing itself and function returning to normal or near normal. Repair of the organ tissue can take days to months, leaving the kidney function abnormal during that time. Many patients with acute kidney damage will respond to supportive care and treatment of the underlying disease and there is no need for hemodialysis. These treatments may include intravenous fluids, antibiotics, and anti-vomiting medications. When the degree of damage is enough to cause marked accumulations of toxins in the body and/or the loss of the ability to make urine, and supportive treatments are not leading to improvement of kidney function, hemodialysis is a treatment consideration.
 If my pet needs hemodialysis, how long does treatment last?
If my pet needs hemodialysis, how long does treatment last?
Hemodialysis does not fix the kidneys. It merely filters the toxins from the blood, making the pet feel better and allowing their kidneys time to heal. The speed at which the kidneys heal vary and depend on the underlying cause as well as variations between individual pets. In the beginning, a pet may need daily treatments. When the patient stabilizes, treatments may be every 2-3 days. When kidney function is improved or the patient is making urine, dialysis ceases and traditional medical treatments continue until the patient goes home. Kidney recovery can take between 2-6 weeks (sometimes months) and patients may need dialysis treatments for 2-4 weeks. In some cases, we can treat pets on an outpatient basis, having them come in every 2 days for treatment. We find most patients only need dialysis for the first 1-2 weeks.
Individual treatment sessions last between 4-12 hours depending in the cause of the kidney dysfunction. Treatment times depend on a number of factors. The initial treatments typically last the longest and become shorter during the course of hospitalization.
How will my pet receive nutrition during treatments?
Most patients with kidney injury or disease will have poor appetites, and as nutrition is very important, many pets will have a feeding tube placed at the time of the hemodialysis catheter placement. An esophagostomy tube is commonly used. Placement of the esophagostomy tube occurs with the patient under general anesthesia. The advantage of an esophagostomy tube is that we can feed a complete, balanced diet that promotes recovery.
Can hemodialysis treat diseases other than kidney disease?
The answer is a resounding, YES! Removal of toxins from the blood can occur with the combined techniques of hemodialysis and hemoperfusion. Hemoperfusion utilizes a special charcoal filter that binds toxins, removing them from the blood. Hemoperfusion has been used successfully to treat toxicities in both dogs and cats.
What is the prognosis?
The prognosis for recovery from acute kidney damage in dogs and cats treated with hemodialysis depends on the cause, extent of renal damage, concurrent disease, and presence of multiple organ system involvement. Based on the published studies, global survival for dogs with severe acute uremia is approximately 50 percent. Survival from infectious (60 percent), hemodynamic and metabolic etiologies (40 percent) was greater than survival from toxic causes (20 percent). The outcome for dogs with acute leptospirosis is especially favorable with 80-90 percent survival with either severe (dialysis-dependent) or milder forms (medically manageable) of acute renal failure (ARF). Reported global survival for cats requiring hemodialysis is 56 percent. Overall, hemodialysis substantially increases the global survival for both dogs and cats with severe acute kidney damage beyond what would be expected with conventional management.
What about chronic kidney disease?
Dogs and cats with chronic kidney disease can undergo long-term hemodialysis. This is similar to people who get hemodialysis 3 times a week for the remainder of their lives. Veterinary patients can experience a very good quality of life. Patients have been treated chronically and still go hiking with their human companions and live amazing lives. We must remember, however, that this is a huge commitment, from an emotional and financial point of view. Not all pets are good candidates. A hemodialysis doctor will perform a detailed review of the case and they will determine if your pet is a candidate for chronic hemodialysis.
Summary
Hemodialysis can be a life-saving procedure for patients with acute kidney injury, allowing patients greater chance of survival. For patients with a treatable underlying disease, hemodialysis is a reasonable consideration for any pet experiencing severe acute kidney disease.
Learn more about Hemodialysis at NorthStar VETS.
Benjamin Davidson, BVSc, MANZCVSc, DACVECC
 Dr. Davidson graduated from the University of Queensland School of Veterinary Science in 1998. He obtained experience as an emergency veterinarian for five years before starting a residency in small animal emergency and critical care at the Cummings School of Veterinary Medicine at Tufts University in 2003. He completed his residency in 2006 and became board certified in emergency and critical care the same year. Dr. Davidson then took on a role as a senior clinician at BluePearl Veterinary Partners in New York City, where he headed the critical care service for ten years. He then headed the critical care and hemodialysis services at BluePearl in Paramus, NJ. Board certified and proficient in all fields of veterinary emergency and critical care, Dr. Davidson’s professional interests include mechanical ventilation, trauma, sepsis and extracorporeal methods of organ support, including hemodialysis, ultrafiltration and membrane oxygenation. Dr. Davidson has authored articles and textbook chapters on the topics of critical care, and routinely lectures to veterinarians.
Dr. Davidson graduated from the University of Queensland School of Veterinary Science in 1998. He obtained experience as an emergency veterinarian for five years before starting a residency in small animal emergency and critical care at the Cummings School of Veterinary Medicine at Tufts University in 2003. He completed his residency in 2006 and became board certified in emergency and critical care the same year. Dr. Davidson then took on a role as a senior clinician at BluePearl Veterinary Partners in New York City, where he headed the critical care service for ten years. He then headed the critical care and hemodialysis services at BluePearl in Paramus, NJ. Board certified and proficient in all fields of veterinary emergency and critical care, Dr. Davidson’s professional interests include mechanical ventilation, trauma, sepsis and extracorporeal methods of organ support, including hemodialysis, ultrafiltration and membrane oxygenation. Dr. Davidson has authored articles and textbook chapters on the topics of critical care, and routinely lectures to veterinarians.
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
Posted in Pets, Veterinary Medicine
Tagged acute kidney injury, Benjamin Davidson, hemodialysis, NorthStar VETS
Leave a comment
From the Client Perspective: Living with IMHA
Ethan joined my family from Glen Highland Farm Rescue on December 26, 2009. I was his 4th home in his short time on this earth of 10 months. No one could figure out how to effectively communicate with him. He was quirky and anxious. But we took a chance on each other and I think he has taught me more than I have taught him.
 I was looking for my next competition dog and I thought Ethan could be it. We did enter the show arena in agility, herding, and lure coursing, but his insecurities would get the better of him and he would “act out.” What people didn’t realize was that he wasn’t giving me a hard time, he was having a hard time. I decided it was best for us to focus on him being comfortable in his own skin. He may not have won any big titles or events, but he is a champion in my eyes.
I was looking for my next competition dog and I thought Ethan could be it. We did enter the show arena in agility, herding, and lure coursing, but his insecurities would get the better of him and he would “act out.” What people didn’t realize was that he wasn’t giving me a hard time, he was having a hard time. I decided it was best for us to focus on him being comfortable in his own skin. He may not have won any big titles or events, but he is a champion in my eyes.
Those who know the story of Ethan know how difficult life was for him, as he was presented with challenges daily. Fear of other dogs, reactivity to motion, cars, bicycles, lights, sounds, ceiling fans – you name it. Together we learned how to conquer his fears, and Ethan finally allowed himself to be happy and content. That’s when we faced his next big battle – IMHA.
In August of 2018, Ethan started to urinate blood and seemed mopey. I knew something was wrong. My other border collie, Shane, was dying of gastric carcinoma, and now Ethan was on the brink of death with a disease I knew nothing about. It was then that I met with Dr. Tammy Anderson of the NorthStar VETS Internal Medicine team. She had previously treated another dog for me. I remembered her being knowledgeable and compassionate. I was terrified at the prospect of losing two precious border collies both within the same week.
 Immune-mediated hemolytic anemia (IMHA) is a condition where the body’s immune system attacks and removes its own red blood cells, leading to severe anemia, an unhealthy yellow coloring of the tissues called jaundice, as well as an assortment of life-threatening complications. Mortality from this condition is high, so veterinarians take an aggressive approach. Multiple blood transfusions and immune-suppressive drugs are needed.
Immune-mediated hemolytic anemia (IMHA) is a condition where the body’s immune system attacks and removes its own red blood cells, leading to severe anemia, an unhealthy yellow coloring of the tissues called jaundice, as well as an assortment of life-threatening complications. Mortality from this condition is high, so veterinarians take an aggressive approach. Multiple blood transfusions and immune-suppressive drugs are needed.
Dr. Anderson promised that she would do all that she could. It was very touch-and-go for a while, but Ethan made it through his first transfusion and eventually became stable enough to be discharged. I believe Dr. Anderson and I spoke several times a week for the first two months after his diagnosis, as she wanted to closely monitor his care.
 A few weeks after his discharge, we took Ethan kayaking down the Delaware River. I sent Dr. Anderson videos and pictures, as I didn’t want to just share the bad, but I wanted to share the good as well. At the end of each call or visit, she would tell me “Enjoy him.” That truly touched my heart, as her sentiment was genuine.
A few weeks after his discharge, we took Ethan kayaking down the Delaware River. I sent Dr. Anderson videos and pictures, as I didn’t want to just share the bad, but I wanted to share the good as well. At the end of each call or visit, she would tell me “Enjoy him.” That truly touched my heart, as her sentiment was genuine.
Over the next few months, we battled skin infections, fluctuating PCV numbers and elevated liver enzymes. And then in February 2019, the biggest fear of IMHA dogs came true – Ethan crashed. A transfusion would be more difficult now, as he would have to be cross-typed and matched. Ethan rejected the first transfusion and things were looking dim. Dr. Anderson was just as upset and concerned as I was. We spoke frankly, and Dr. Anderson took the time to explain everything thoroughly and with compassion.
 We made a joint decision to try one more time. If it didn’t work, we at least would know that we tried our best. The second transfusion worked! But we both knew Ethan was very fragile now. We then tried several different types of medication and that seemed to work. Our weekly/bi-weekly visits continued and Ethan became like “Norm” from the show “Cheers.” Ethan would walk into the hospital and EVERYONE knew his name. This made him light up! He gets showered with attention and cookies whenever he goes into the back for his tests and bloodwork.
We made a joint decision to try one more time. If it didn’t work, we at least would know that we tried our best. The second transfusion worked! But we both knew Ethan was very fragile now. We then tried several different types of medication and that seemed to work. Our weekly/bi-weekly visits continued and Ethan became like “Norm” from the show “Cheers.” Ethan would walk into the hospital and EVERYONE knew his name. This made him light up! He gets showered with attention and cookies whenever he goes into the back for his tests and bloodwork.
 The staff at NorthStar has been wonderful with Ethan and have made us both feel at home. Several months went by until June of 2019 when Ethan got infected elbow hygromas and was septic. Again, Dr. Anderson pulled off yet another miracle and Ethan survived this as well. All throughout Ethan’s ordeals, Dr. Anderson remained genuinely concerned, knowledgeable, compassionate, but also grounded in reality. We told Ethan that he needed a new hobby, and jokingly said that he is on the “I’m Not Dead Yet” Tour. We are hoping the tour continues for the next few years! We have had a few more scares, such as bilateral calcium deposits and bizarre bony growths in his carpus, but Ethan continued to improve every week. He was an IMHA warrior.
The staff at NorthStar has been wonderful with Ethan and have made us both feel at home. Several months went by until June of 2019 when Ethan got infected elbow hygromas and was septic. Again, Dr. Anderson pulled off yet another miracle and Ethan survived this as well. All throughout Ethan’s ordeals, Dr. Anderson remained genuinely concerned, knowledgeable, compassionate, but also grounded in reality. We told Ethan that he needed a new hobby, and jokingly said that he is on the “I’m Not Dead Yet” Tour. We are hoping the tour continues for the next few years! We have had a few more scares, such as bilateral calcium deposits and bizarre bony growths in his carpus, but Ethan continued to improve every week. He was an IMHA warrior.
 Today, as of February 2020, Ethan is off prednisone and we are slowly continuing to taper him off the other immunosuppressants. He has gained weight, his coat has come back in full, and is lush and curly. He is active playing ball, running in the yard, and that spark is back in his eyes. We truly appreciate all that NorthStar VETS and Dr. Tammy Anderson have done for us. This has certainly been an emotional rollercoaster, but the one thing that has remained steadfast is Dr. Anderson’s devotion to her patient’s care.
Today, as of February 2020, Ethan is off prednisone and we are slowly continuing to taper him off the other immunosuppressants. He has gained weight, his coat has come back in full, and is lush and curly. He is active playing ball, running in the yard, and that spark is back in his eyes. We truly appreciate all that NorthStar VETS and Dr. Tammy Anderson have done for us. This has certainly been an emotional rollercoaster, but the one thing that has remained steadfast is Dr. Anderson’s devotion to her patient’s care.
Learn more about the Internal Medicine service at NorthStar VETS
 Tammy Anderson, DVM, DACVIM
Tammy Anderson, DVM, DACVIM
Dr. Anderson is a New Jersey native who received her veterinary medical degree from Ohio State University in 1995. She completed her small animal internship at Michigan State University in 1996, and her residency in small animal internal medicine at the University of Tennessee in 1999. She remained at UT as an assistant professor of small animal medicine until 2001, when she returned to New Jersey and entered private practice. Dr. Anderson joined NorthStar VETS in 2004.
Posted in Pets, Pets, Veterinary Medicine
Tagged Dr Tammy Anderson, IMHA, Internal Medicine, NorthStar VETS
Leave a comment